# 5945
We’ve looked at a connection between enhanced flu mortality and bacterial co-infections many times in the past, most recently last September in mBio: Lethal Synergism of H1N1 Pandemic Influenza & Bacterial Pneumonia.
In that study scientists at NIAID and the Institute for Systems Biology (ISB) infected experimental mice with both seasonal flu and the 2009 H1N1 pandemic flu, and after 48 hours exposed some of them to Streptococcus pneumoniae, one of the main causes of pneumonia.
Mice that were exposed only to the two flu strains showed expected flu symptoms, but all survived.
Mice that were exposed to seasonal flu and S. pneumoniae experienced minor lung damage, but once again, all survived.
But all of the mice infected with the pandemic H1N1 virus, and S. pneumoniae showed severe weight loss, lung damage, and 100% mortality
Indicating that pandemic H1N1, more than seasonal flu, exacerbated an S. pneumoniae co-infection.
In 2008, we saw a study in The Journal of Infectious Diseases by Morens, Taubenberger, and Fauci that looks at the role of bacterial pneumonia in the high death toll of 1918 (see Viral-Bacterial Copathogenesis).
An excerpt from their study reads:
Conclusions. The majority of deaths in the 1918–1919 influenza pandemic likely resulted directly from secondary bacterial pneumonia caused by common upper respiratory–tract bacteria.
Less substantial data from the subsequent 1957 and 1968 pandemics are consistent with these findings. If severe pandemic influenza is largely a problem of viral-bacterial copathogenesis, pandemic planning needs to go beyond addressing the viral cause alone (e.g., influenza vaccines and antiviral drugs).
2008 also saw additional studies published in the CDC’s EID Journal that looked at the synergy between pandemic flu and bacterial pneumonia, including:
Brundage JF, Shanks GD. Deaths from bacterial pneumonia during 1918–19 influenza pandemic. Emerg Infect Dis. 2008 Aug;
Ravindra K. Gupta,* Robert George, and Jonathan S. Nguyen-Van-Tam Bacterial Pneumonia and Pandemic Influenza Planning Emerg Infect Dis. 2008 Aug;
Shanks and Brundage found, for instance, that during the 1918 pandemic 5% of the deaths attributed to the 1918 pandemic occurred in the first 3 days of infection, while the median time from illness onset to death was 7–10 days, with many deaths occurring >2 weeks after initial symptoms..
Which they believed was more indicative of death due to secondary bacterial infection than directly from a flu virus, or a cytokine storm response (see Influenza's One-Two Punch).
These studies, along with a number of others, have enforced the idea that pneumococcal vaccines like PCV7 Pneumococcal Vaccine Would Save Lives In A Pandemic.
Given this past research, it shouldn’t come as a terrible surprise that a study that appears today in the journal Pediatrics found, among other things, that a co-infection with MRSA was associated with a higher mortality rate among healthy kids infected with the 2009 H1N1 pandemic virus.
First a link to the study, and an excerpt from the abstract, then I’ll be back with more.
Critically Ill Children During the 2009–2010 Influenza Pandemic in the United States
Adrienne G. Randolph,Frances Vaughn, Ryan Sullivan, Lewis Rubinson, B. Taylor Thompson, Grace Yoon, Elizabeth Smoot, Todd W. Rice, Laura L. Loftis, Mark Helfaer,Allan Doctor, Matthew Paden, Heidi Flori, Christopher Babbitt, Ana Lia Graciano, Rainer Gedeit, Ronald C. Sanders, John S. Giuliano, Jerry Zimmerman, Timothy M. Uyeki
(EXCERPT)
Overall, 71 (8.5%) of the patients had a presumed diagnosis of early (within 72 hours after PICU admission) Staphylococcus aureus coinfection of the lung with 48% methicillin-resistant S aureus (MRSA). In multivariable analyses, preexisting neurologic conditions or immunosuppression, encephalitis (1.7% of cases), myocarditis (1.4% of cases), early presumed MRSA lung coinfection, and female gender were mortality risk factors. Among 251 previously healthy children, only early presumed MRSA coinfection of the lung (relative risk: 8 [95% confidence interval: 3.1–20.6]; P < .0001) remained a mortality risk factor.
Conclusions: Children with preexisting neurologic conditions and immune compromise were at increased risk of pH1N1-associated death after PICU admission. Secondary complications of pH1N1, including myocarditis, encephalitis, and clinical diagnosis of early presumed MRSA coinfection of the lung, were mortality risk factors.
The entire study is behind a pay wall, but we’ve a lengthy press release available with considerable detail.
Why Did Healthy Children Fall Critically Ill in the 2009 H1N1 Flu Pandemic?
Largest study to date finds co-infection with MRSA increased death risk 8-fold; flu vaccination urged
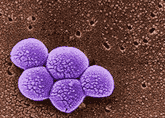
BOSTON, Nov. 7, 2011 /PRNewswire-USNewswire/ -- During the 2009 H1N1 influenza pandemic, many previously healthy children became critically ill, developing severe pneumonia and respiratory failure, sometimes fatal. The largest nationwide investigation to date of influenza in critically ill children, led by Children's Hospital Boston, found one key risk factor: Simultaneous infection with methicillin-resistant Staphylococcus aureus (MRSA) increased the risk for flu-related mortality 8-fold among previously healthy children.
Moreover, almost all of these co-infected children were rapidly treated with vancomycin, considered to be appropriate treatment for MRSA. The fact that they died despite this treatment is especially alarming given the rising rates of MRSA carriage among children in the community.
"There's more risk for MRSA to become invasive in the presence of flu or other viruses," says study leader Adrienne Randolph, MD, MsC, of the Division of Critical Care Medicine at Children's Hospital Boston. "These deaths in co-infected children are a warning sign."
The researchers hope their findings, published November 7 by the journal Pediatrics, (eFirst pages) will promote flu vaccination among all children aged 6 months and older. (No flu vaccine is currently available for children younger than 6 months.)
As we’ve discussed before, a small percentage of the population is known to carry either MRSA or non-resistant S. aureus in their nasal cavities.
This from the CDC:
Definition of MRSA
While 25% to 30% of people are colonized* in the nose with staph, less than 2% are colonized with MRSA (Gorwitz RJ et al. Journal of Infectious Diseases. 2008:197:1226-34.).
*Colonized:
When a person carries the organism/bacteria but shows no clinical signs or symptoms of infection. For Staph aureus the most common body site colonized is the nose.
While 2% doesn’t sound like a lot, there are signs that number may be increasing. Once considered primarily a hospital acquired infection, CA-MRSA (community acquired) is growing in incidence.
For instance, In Firefighters & Paramedics At Greater Risk Of MRSA and Firefighters & MRSA Revisited we looked at research showing a 10x’s greater incidence of MRSA colonization (20%) among a sampling of firefighters tested in Washington State.
Most of the time our immune systems keep these bacteria in check, and we display no outward signs of infection.
But when our immune systems are weakened, such as when we are stricken by influenza, these resistant bacteria can suddenly bloom and become invasive.
Again, from the Press Release:
Influenza appears to suppress the immune response, making children who are already colonized more susceptible to invasive bacterial disease.
"Previously, MRSA has not been considered a common cause of pneumonia in kids but this may be changing," Randolph says. "It's likely that flu and other viral infections let MRSA invade and that there's some synergistic reaction between flu and these bacteria."
While this study specifically links MRSA to bad outcomes among children with pandemic H1N1, the 2008 study by Shanks and Brundage found that during the 1918 pandemic:
. . . the bacteria most often recovered from the sputum, lungs, and blood of pneumonia patients, alive or dead, were common colonizers of the upper respiratory tracts of healthy persons, i.e., Hemophilus influenzae, Streptococcus pneumoniae, S. pyogenes, and/or Staphylococcus aureus.
Whether it is the routine carriage of bacteria in our respiratory system, or the make up of the microflora in our gut biome, scientists are increasingly linking our health, and the progression and outcome of some diseases, to our individual body’s ecosystem.
Which may explain, at least partially, why 99 out of 100 people can catch the flu and recover quickly and without incident, while an unlucky 1% may endure a serious and sometimes fatal illness.
The authors of today’s study advise:
Physicians seeing children with serious lower-respiratory-tract disease during flu season are urged to give early antiviral treatment (Tamiflu or zanamivir [Relenza]) and antibiotics covering MRSA and other flu-associated bacteria, even before suspected infections are confirmed in the lab, the researchers say.
But other approaches are urgently needed. "MRSA is hard to develop a vaccine against – researchers have been trying since the 1960s and have been unsuccessful," says Randolph. "So the only way to prevent these severe complications is to get everyone vaccinated against the flu, and do more studies of MRSA colonization so we can prevent it in the community and in kids."
Further evidence, as if we needed it, that influenza and its complications can be complex, difficult, and occasionally deadly foes.
Related Post:
Widget by [ Iptek-4u ]